What is SIBO?
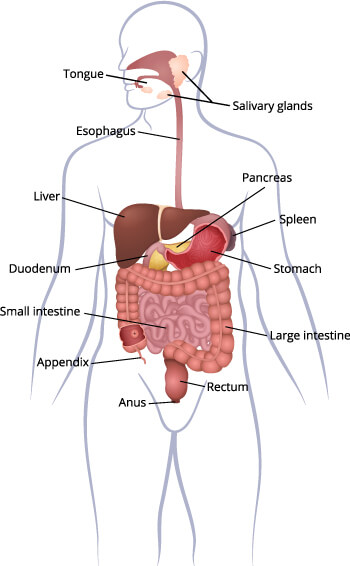
It is defined as having either an increased number of, or abnormal types of bacteria in the small intestine. It is normal and healthy to have bacteria throughout the gastro-intestinal tract (gut) with the greatest number and diversity found in the large intestine. When there is an excess of bacteria in the small intestine this may result in:
- feeling of bloating or abdominal discomfort or actual abdominal distension due to the over-production of gas produced by the digestion of food by bacteria
- interference with digestion and absorption of nutrients that may in serious cases lead to some nutrient deficiencies
- damage to the lining of the small intestine that causes inflammation and may produce symptoms mediated by an imbalanced immune system that seem apparently unrelated to the gut
What are the symptoms of SIBO?
SIBO can therefore present with a variety of different symptoms, which are not unique to SIBO and make it hard to identify. Most doctors are not familiar with how to test for it or how to address it. The following are symptoms that are most commonly associated with SIBO:
- bloating, with or without abdominal distension
- flatulence
- abdominal discomfort
- unexplained diarrhoea
- constipation or alternating diarrhoea and constipation
- nutrient deficiencies – anaemia
- skin conditions – acne rosacea
- brain ‘fog’
There is an overlap with symptoms that are also common in patients with medically diagnosed IBS and research indicates that SIBO may be part of the pathogenesis of IBS (1,2) ie IBS symptoms may be due to underlying SIBO.
What are the causes of SIBO?
SIBO may occur because bacteria have been displaced from the oral cavity or from the colon and/or because conditions in the small intestine promote colonization and growth such as reduced acidity (pH) or due to availability of foods that the bacteria like to feed on.
The root causes of SIBO are therefore quite diverse and require an understanding of diet and lifestyle habits, critical life events and health history. There are multiple possible causes that may include:
- Anatomical abnormalities – genetic anomalies or resulting from previous abdominal surgery such as adhesions
- Low Stomach acid – gastric acid in the stomach kills many bacteria and provides an effective barrier between the mouth and the small intestine. What can cause low stomach acid?
- Use of antacids such as PPIs (proton pump inhibitors) taken for conditions such as acid reflux, heartburn, gastroesophageal reflux disease (GERD), ulcers, laryngopharyngeal reflux (LPR), gastritis and H.pylori infections.
- Ageing – we produce lower levels of stomach acid as we get older
- Bile and Pancreatic Enzyme deficiencies – normal production of these enzymes promotes digestion and may limit growth of bacteria in the small intestine. What can cause these deficiencies?
- Bile deficiency that may be caused by dysfunction of the gall bladder and/or liver
- Stomach contents empty into the small intestine and create a mildly acidic pH which stimulates the secretion of pancreatic enzymes and bile, so here again low stomach acid may also affect pancreatic enzyme secretion
- The overgrowth of bacteria that leads to SIBO may itself cause digestive enzyme deficiency, including de novo Lactose and Fructose intolerance
- Chronic stress, medications or food insensitivities may also cause lower production of digestive enzymes
- Poor motility – which relates to how long it takes for food, bacteria and toxins to be moved along and out of the stomach and small intestine. It is governed by the migrating motor complex (MMC) and takes place during the fasting period between meals. This is not to be confused with constipation. What can cause low motility?
- Snacking or eating often between meals can inhibit the MMC
- Timing of eating during the day
- Opiate pain medications eg codeine
- Certain other conditions such as Parkinson’s disease, diabetes, hypothyroidism, hypermobility
SIBO is likely to be as a result of one of the conditions above. If the root cause is addressed, then reoccurrence may also be avoided.
How I can help?
Clinical assessment:
Functional testing:
Functional testing will be recommended in order to ascertain the presence and nature of SIBO. These include breath tests that you can do at home, as well as stool testing.
Recommendations:
Follow ups:
Book a call with me to find out how my approach could help you live a 'normal' life
In this call we will discuss your symptoms and brief health history and I will explain how I would approach working with you. You can decide whether I am the right person to work with you.
References
- Ford AC, Spiegel BMR, Talley NJ, Moayyedi P. Small Intestinal Bacterial Overgrowth in Irritable Bowel Syndrome: Systematic Review and Meta-analysis. Vol. 7, Clinical Gastroenterology and Hepatology. W.B. Saunders; 2009. p. 1279–86.
- Ghoshal UC, Shukla R, Ghoshal U. Small intestinal bacterial overgrowth and irritable bowel syndrome: A bridge between functional organic dichotomy. Vol. 11, Gut and Liver. Joe Bok Chung; 2017. p. 196–208.